Top 30 Problems in Healthcare
This blog explores the most pressing challenges facing the healthcare system today, from access and equity issues to technological barriers and public health concerns.
Healthcare is a fundamental human right, yet millions around the world lack access to quality care. From skyrocketing costs to systemic inequalities, the healthcare system faces numerous challenges that demand urgent attention. In this post, we list the top 30 problems in healthcare, organized into key areas.
Key Healthcare Challenges
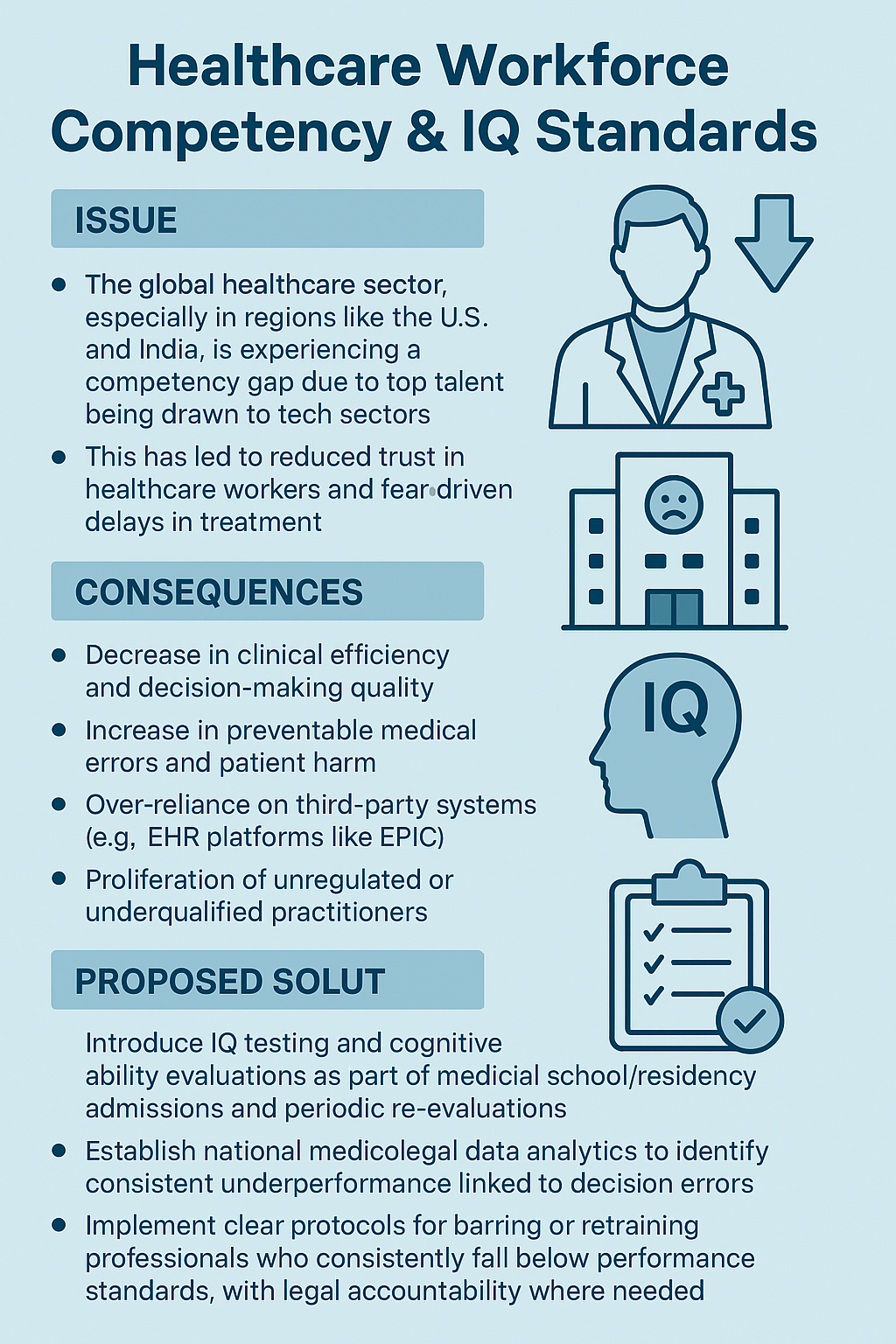
1. Low IQ of healthcare workers
In many countries, especially the English speaking countries like India to United States, healthcare workers got replaced by low IQ counterparts due to talent poaching by the global tech sector, causing competency and ethical hardship. This often forces patients to delay or skip necessary treatments out of fear, worsening health outcomes.
This creates incompetent inefficient healthservices leading to more medical death and more third party interfernce like EPIC or EHR. This leads to more quackery and prolonged workhours lasting more than 80 hours per week. Main cause is influx of women in healthcare and unchecked minorities from established low IQ demography.
Hospital adminstration and Government have been going out of their own way to replace female doctors and minority doctors with native male nursepractitioners and technicians over the past decades
Solutions:
- IQ testing of medical students and residents.
- Banning low IQ doctors from practice after completion of medschool/residency through stringent medicolegal framework that targets data collection and analysis of their patients.
- Quick action to place those who default on serious medicolegal cases in jail or bar them from practice without any second chance.
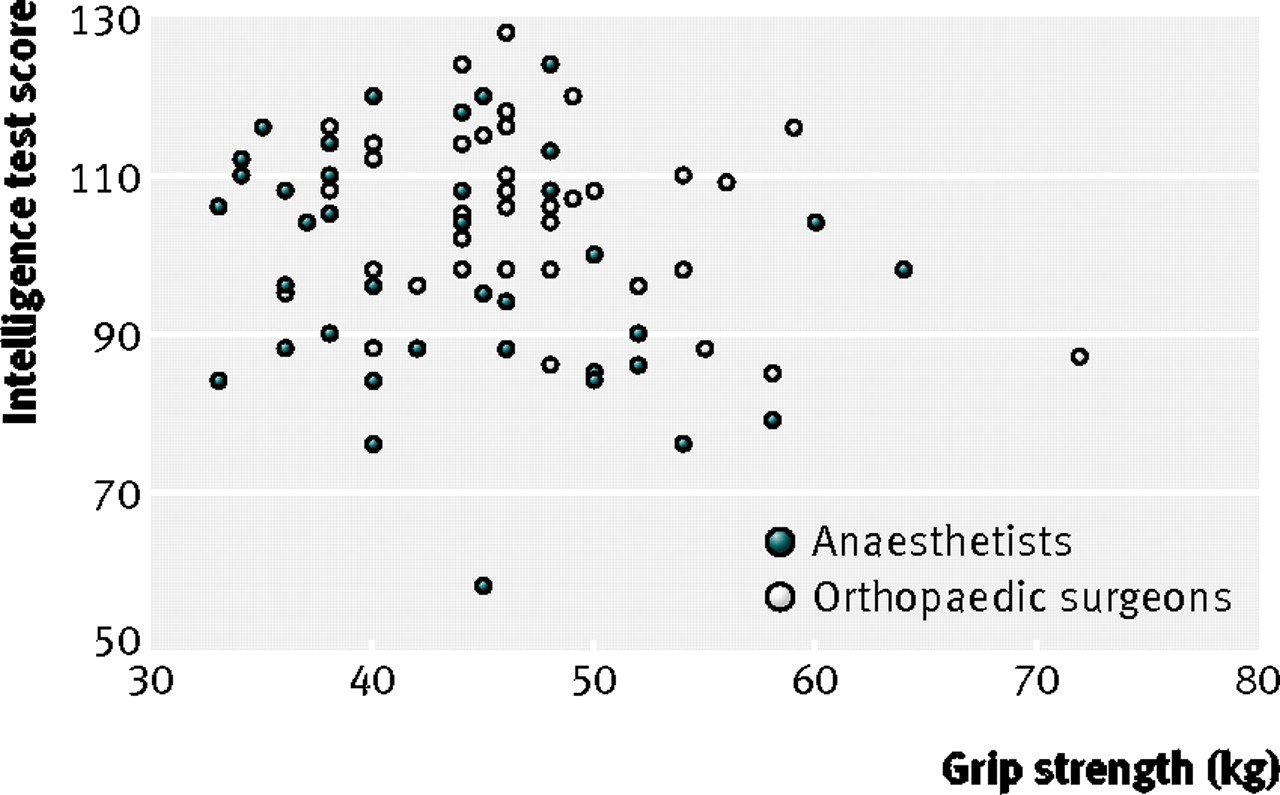
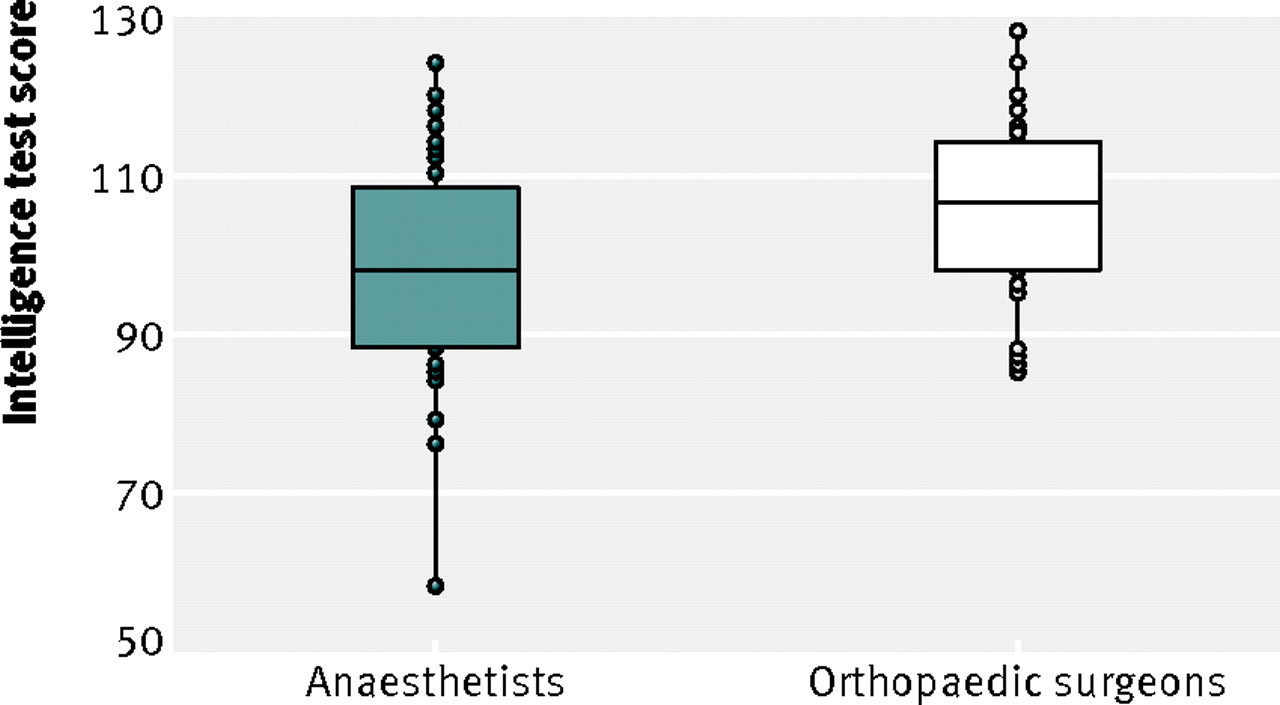
Look at what happened when all high IQ males moved from medicine to tech
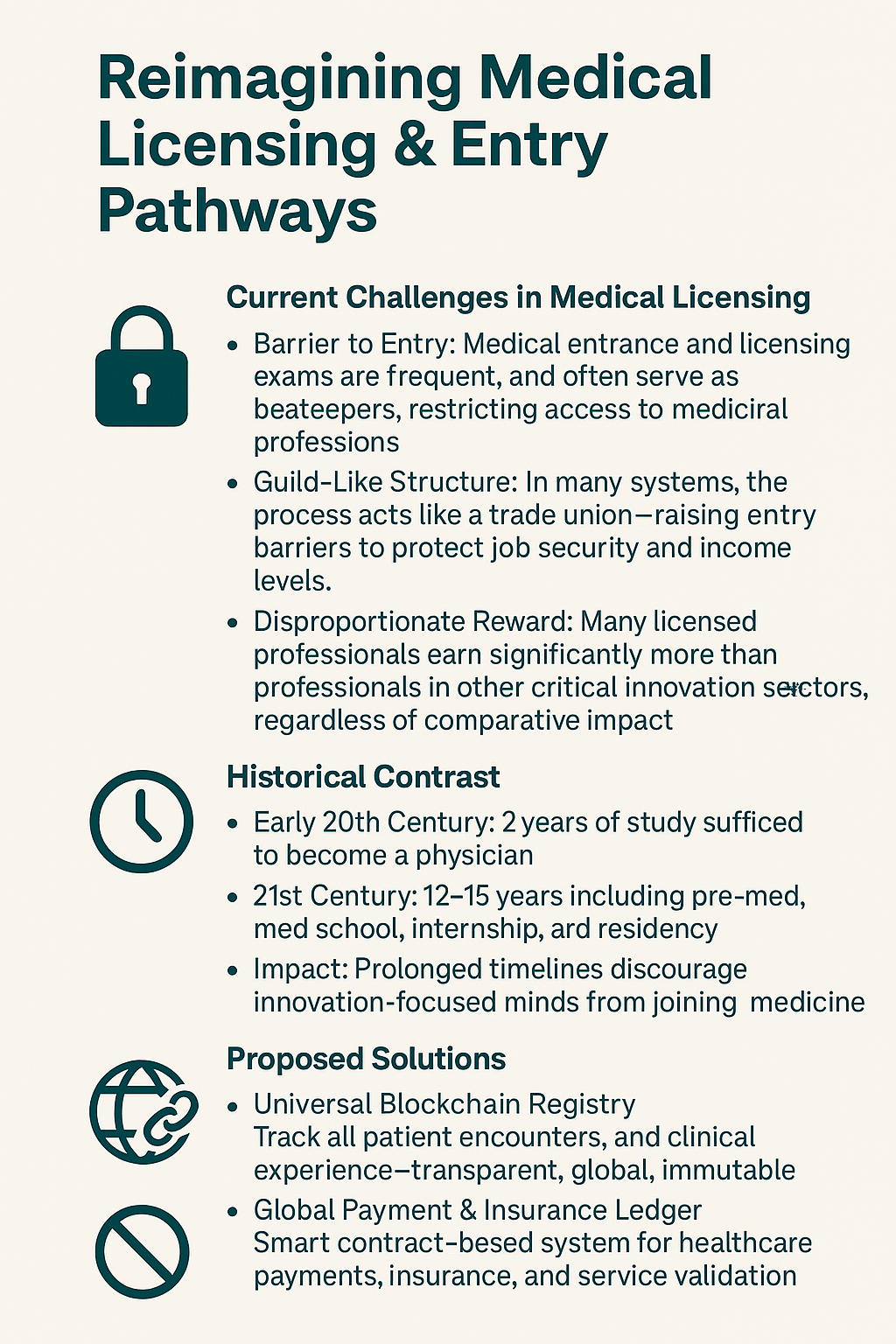
2. Medical licensing, boards and college entry exams
Medical entry exams are frequent, unecessary and exist to limit entry of laymen to the guild of doctors. Its a trade union and barrier to enter the trade union. Its an evil strategy to get higher salary. All across the world the most incompetent doctor with a medical license earns more than a CEO or biotech founder next to him.
This led to higher demand for becoming a doctor hence needing more barrier of entry to practice. In the beginning of 20th century, it took only 2 years of study to become a physician and now it takes 4 years pre-med, 4 years medschool, 1 year internship, 3-6 years of residency to practice medicine.
Solutions:
- universal block chain to tally medical encounters between patients, students, residents and doctors.
- universal payment system and insurance on blockchain
- remove all international medical licensing exams like USMLE, PLAB, KMLE, NEET-PG for residents/consultants of other countries
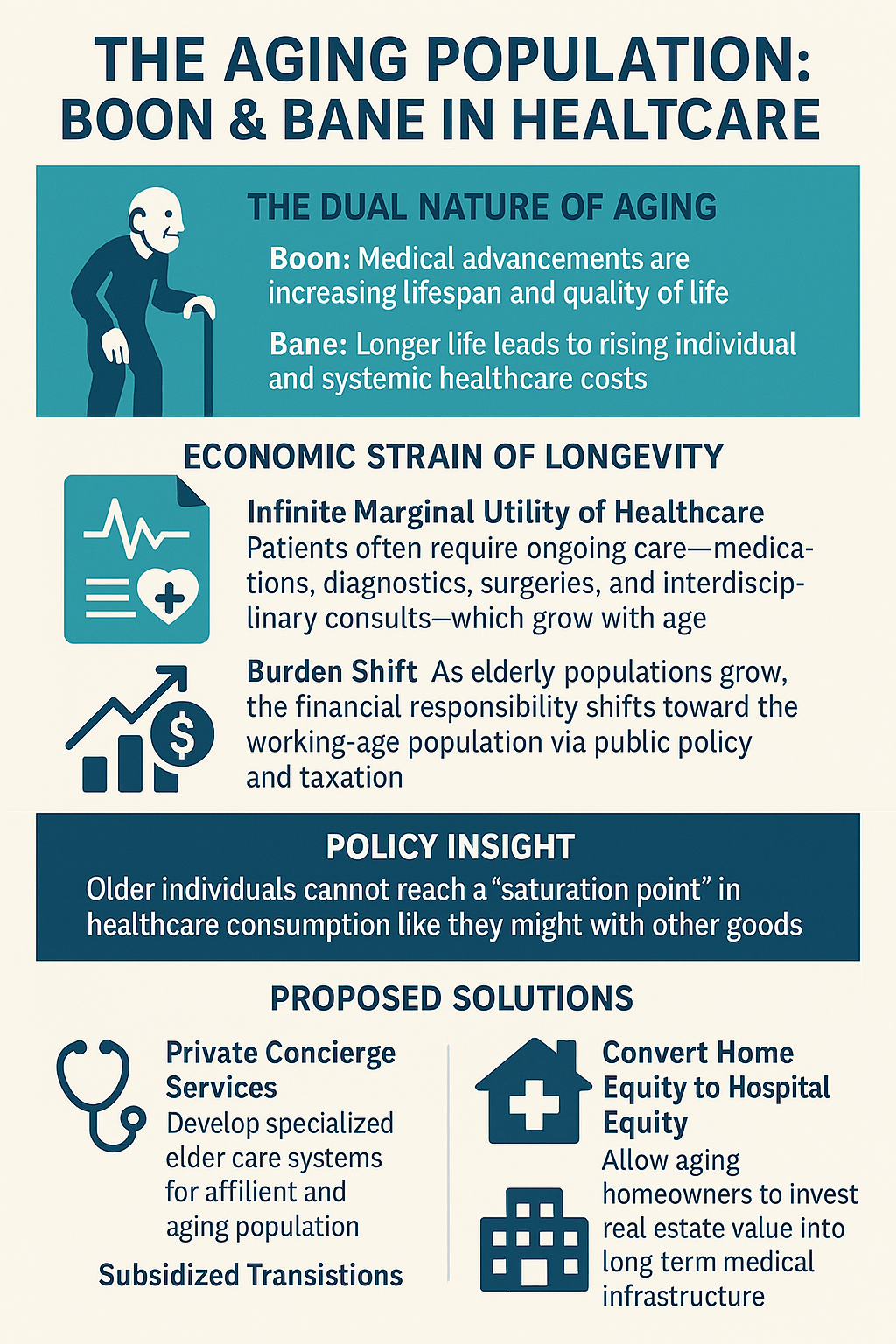
3. Rising age of population - boon and a bane
Longer the patients live, more expensive its for them and the healthcare system. This leads to higher redistribution of healthcare expenses. Healthcare expenses have "infinite marginal utility" meaning it cant be continually used by same person without satiating their healthcare needs or apetite. Example; a heart patient will not stop at heart medication, he will take scans, multiple visits, preventive visits, heart surgery, interdisciplinary visits and the list grows as he age more.
This leads to expenses unbearable to the older demography and as more people age into elderly population, the demand for their healthcare rises. This leads to public policy and voting causing the youngsters to bear the cross of elderly health expenses.
Solutions:
- Private concierge for senior citizens and rich citizenes
- criminalising non cohabitation of elderly with their kids and vice versa
- turn home equity into hospital equity
- subsidise homeowners who wants to sell homes to build hospitals
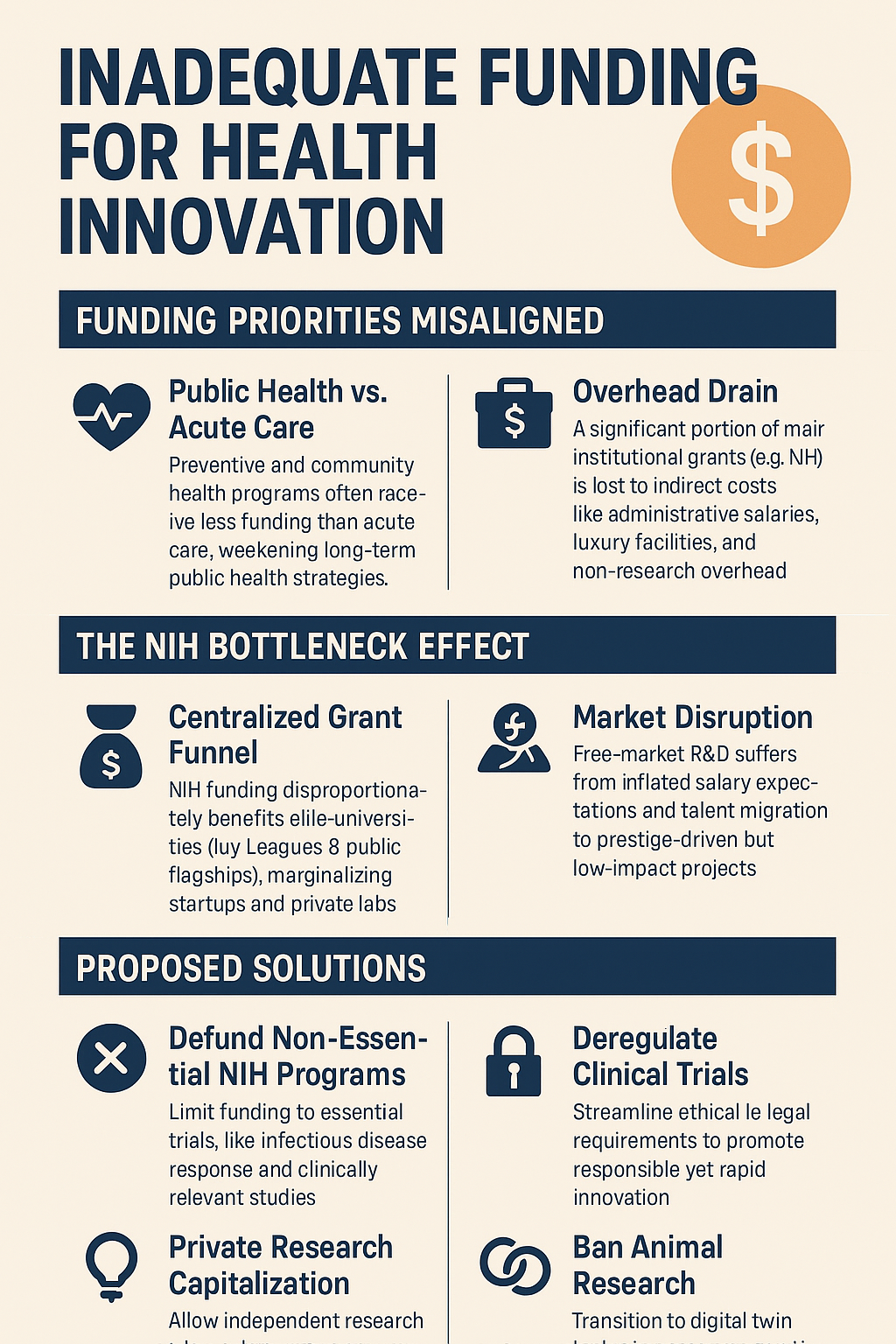
4. Inadequate funding for health initiatives
Public health programs often receive less funding than acute care, limiting disease prevention efforts. This undermines community health strategies. NIH funding has destroyed all public and private health initiatives by "indirect costs" that goes to administration, setting up 5star hotel like instituitions on prime real estate and paying multimillion salaries to doctors,researchers and deans.
NIH funding also funnelled 2 to 10 times more necessary funds to public university and private ivy leageus for research purposes which priced out ALL other private research labs to R&D startups from free market. This led to over expectations of Researcher and Doctor Salaries creating worst hiring for everyone else. This also attracted all global biomedical-tech talents to ivy leagues and USA to waste their talents doing useless NIH funded rat and preclinical studies to prove outdated knowledge or political agenda.
Solutions:
- Stop all NIH funding to ivy leagues and government research labs that are non essentials (thats not infectious disease clinicaltrials)
- Let research labs privately raise money to fund preclinical and clinical research
- Remove as many regulations set on doing clinical trials and other forms of research
- ban animal research and move to more efficinet digital twin technology research
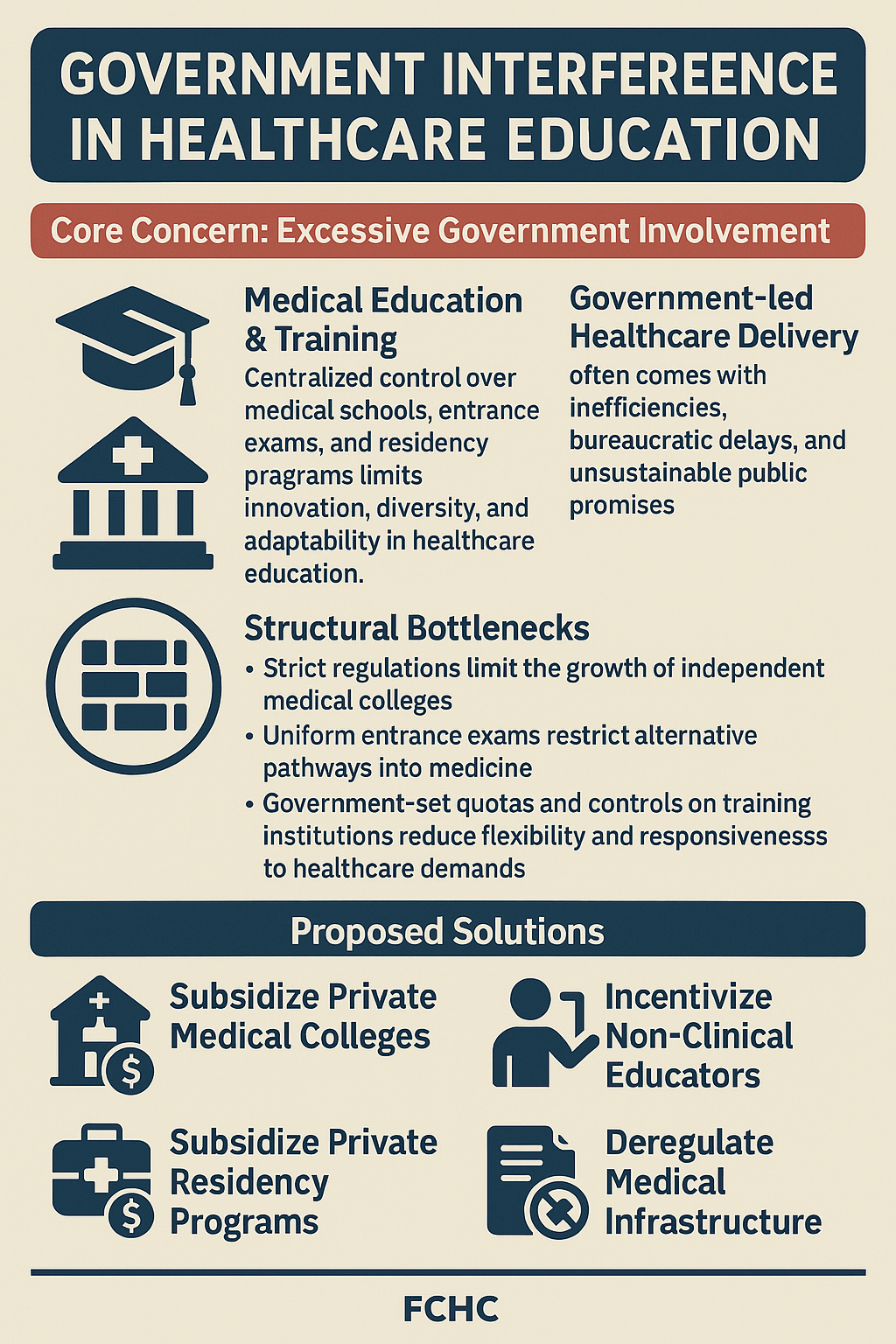
5. Government Interferance in healthcare
Government shouldnt be involved in medical education, medical residency programs or healthcare provision/promises. Government shouldnt be involved in medical school or residency entrance exams.
Solutions:
- Subsidise construction of private medical colleges
- Subsidise construction of private residency colleges
- Subsidise hiring of non clinical tutors
- Remove as many regulations regarding construction and management of medical colleges
6. High cost of healthcare, Non-Profit healthcare organisations
In many countries, especially the United States, healthcare costs are prohibitively high, causing financial hardship. This often forces individuals to delay or skip necessary treatments, worsening health outcomes. Its caused by "non-profit hospital conglomerate", over regulation, government interferance, third party interference and shortage of redistributed medical doctors.
The CEO of American Heart Association earns 4 million USD and AHA has an ARR of closr to one billion, most of which goes to fill the salary of its organisation beurocrats upto 500 million USD. The non-profit hospitals all across the world have tax exemption to store most of their wealth and can afford to pay their attending and consultants upto 900,000 USD per year with their CEOs earning upto multimillion salary package.
Solutions:
- Liberalise medical tests - let patients pick additional tests without prior authorisation of docs or third party
- Allow maximum medical tourism and subsidise medical tourism for patients
- Allow medical consultants and attendings of developing nations to serve in rural areas of developed countries
- Allow curriculum to teach medicalstudents and doctors how to run a business, bigpharma and insurance company
- Allow medical students and doctors to be taught how to design and patent medical devices and softwareas
- Shorten the medical education curriculum to 2 years of medschool and 2 years of residency. Remove internship.
- AI guided matching of correct patient to correct doctor skipping referrals from GP or other specialists
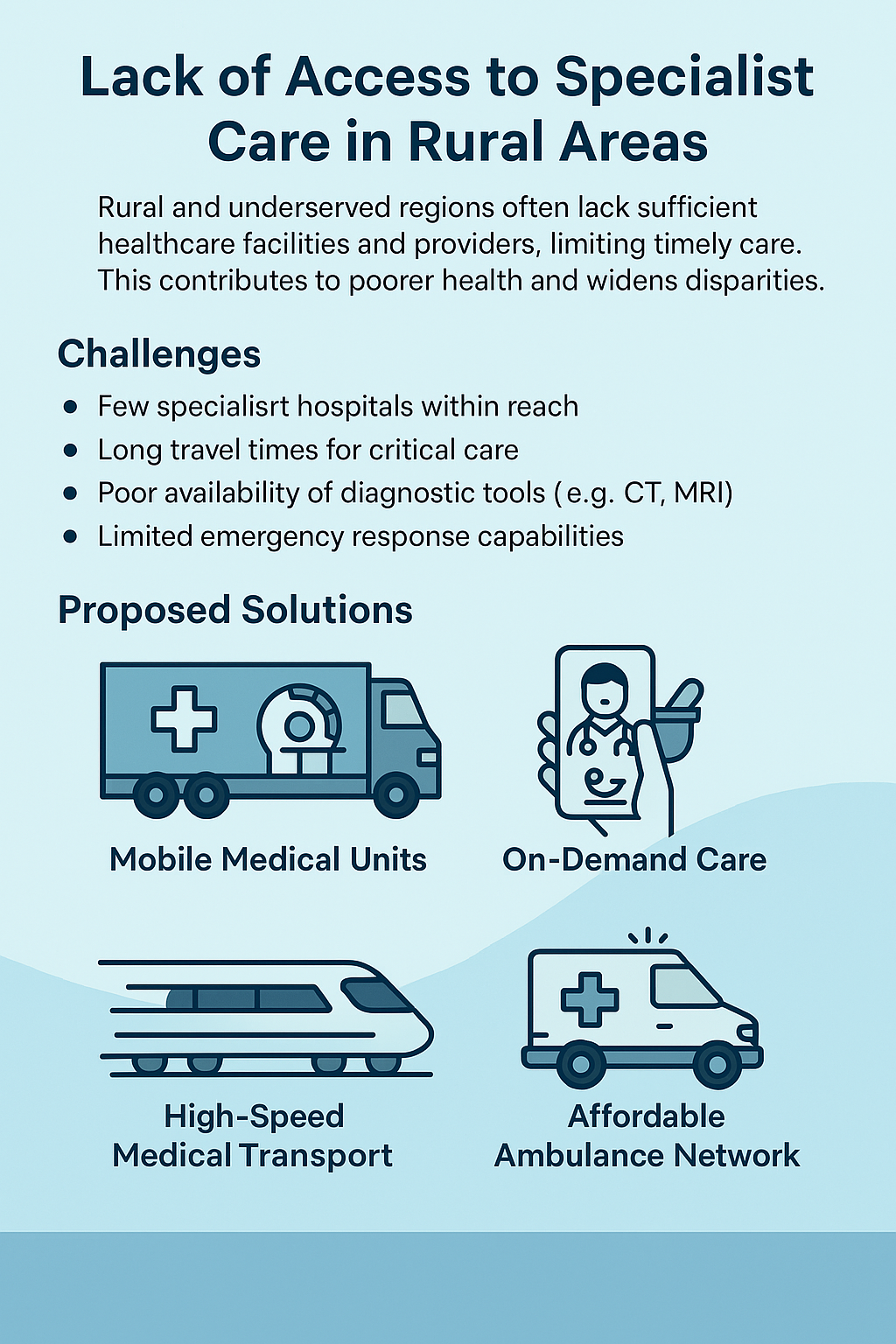
7. Lack of access to specialist care and equipments, especially in rural areas
Rural and underserved regions often lack sufficient healthcare facilities and providers, limiting timely care. This contributes to poorer health and widens disparities.
Solutions:
- Portable CT, MRI, Operation theatre on trailer trucks
- Home delivery of medicines and doctors on demand
- Bullet trains and faster transport for elderly
- Cheaper and quicker ambulance services
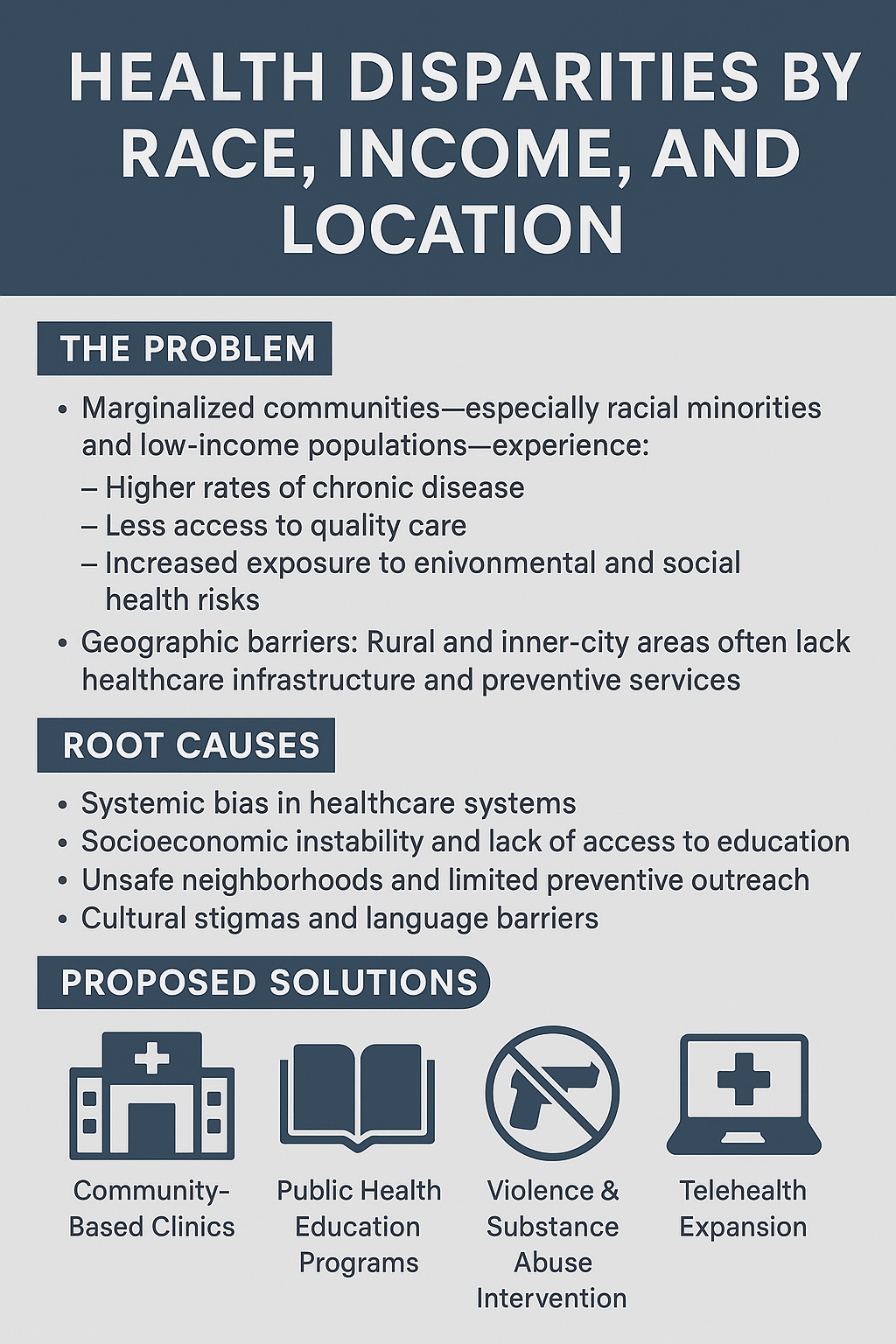
8. Health disparities based on race, income, or location
Systemic inequalities mean marginalized groups frequently receive substandard care, perpetuating cycles of poor health. This reflects deep-rooted social and economic divides.
Solutions:
- Avoiding drug abuse in minority community
- Avoiding prostituition in minortiy community
- Avoiding gun violence in minority community
- Avoiding unsolicited sex and hookup culture in minority community
- Policing more minority areas and more mental health rehabs nearby them
9. Limited access to affordable medications
High drug prices hinder treatment, especially for chronic conditions, leading to non-adherence and declining health. This is a significant barrier to effective care. This led to series of 'medication' insurance called pharmacy benefit manager (who risk pools expensive medications into cheaper medications, inflating cost of cheap ones), medicaid and medicare.
Solutions:
- Importing generic medicines
- Moving pharmaceutical manufacturing to developing countries
- Allowing more competition in drug development and manufacturing
- Implementing price controls on essential medications
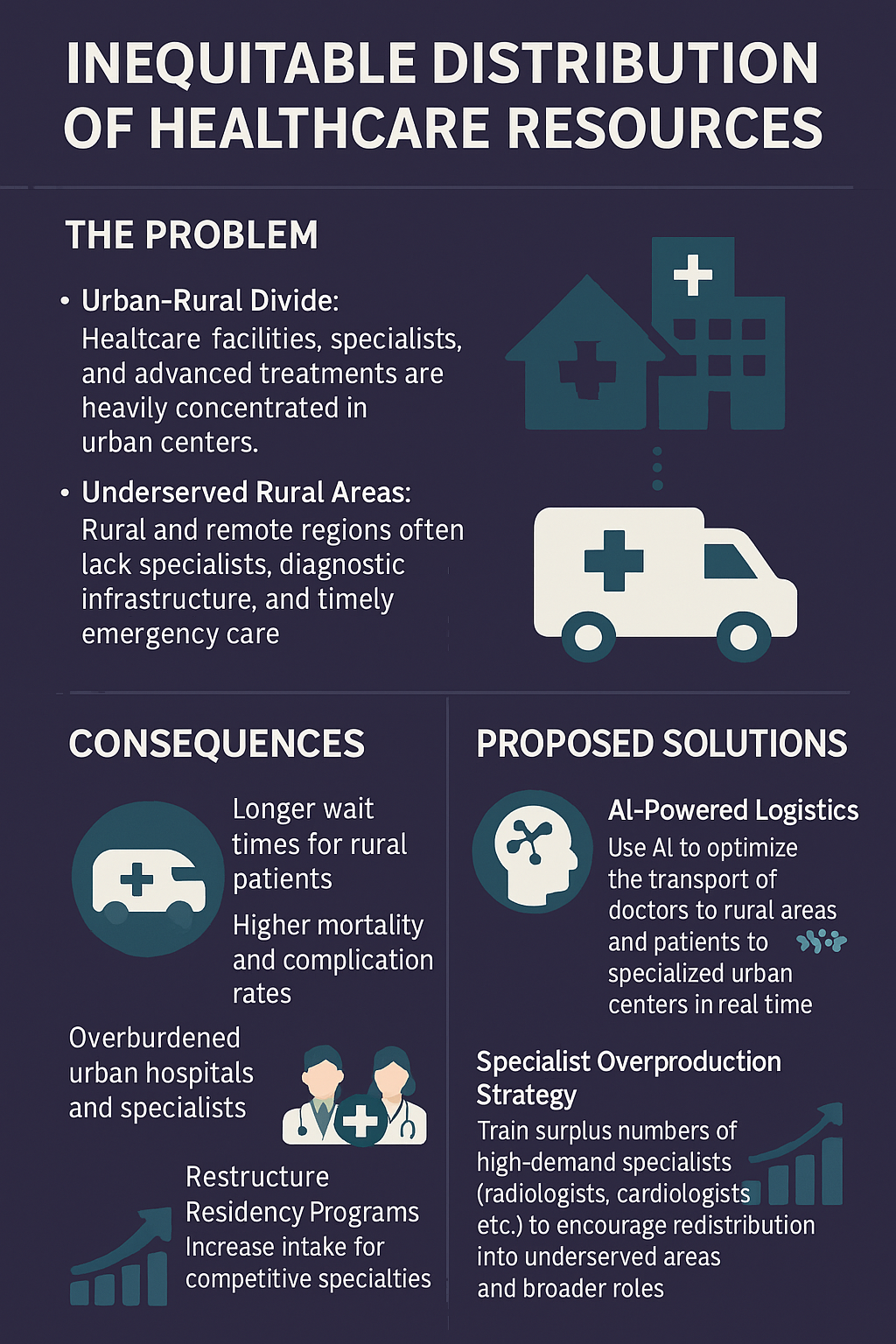
10. Inequitable distribution of healthcare resources
Resources like hospitals and specialists are often concentrated in urban areas, leaving rural communities underserved. This imbalance exacerbates access issues.
Solutions:
- more AI powered logistics to move doctors to rural and patients to urban
- overproduce radiologists,dermatologists , neurosurgeons, cardiologists and CTsurgeons to make them redistribute
- overproduce high medicalstudent demand medical residency programs to push them to take up other specialties
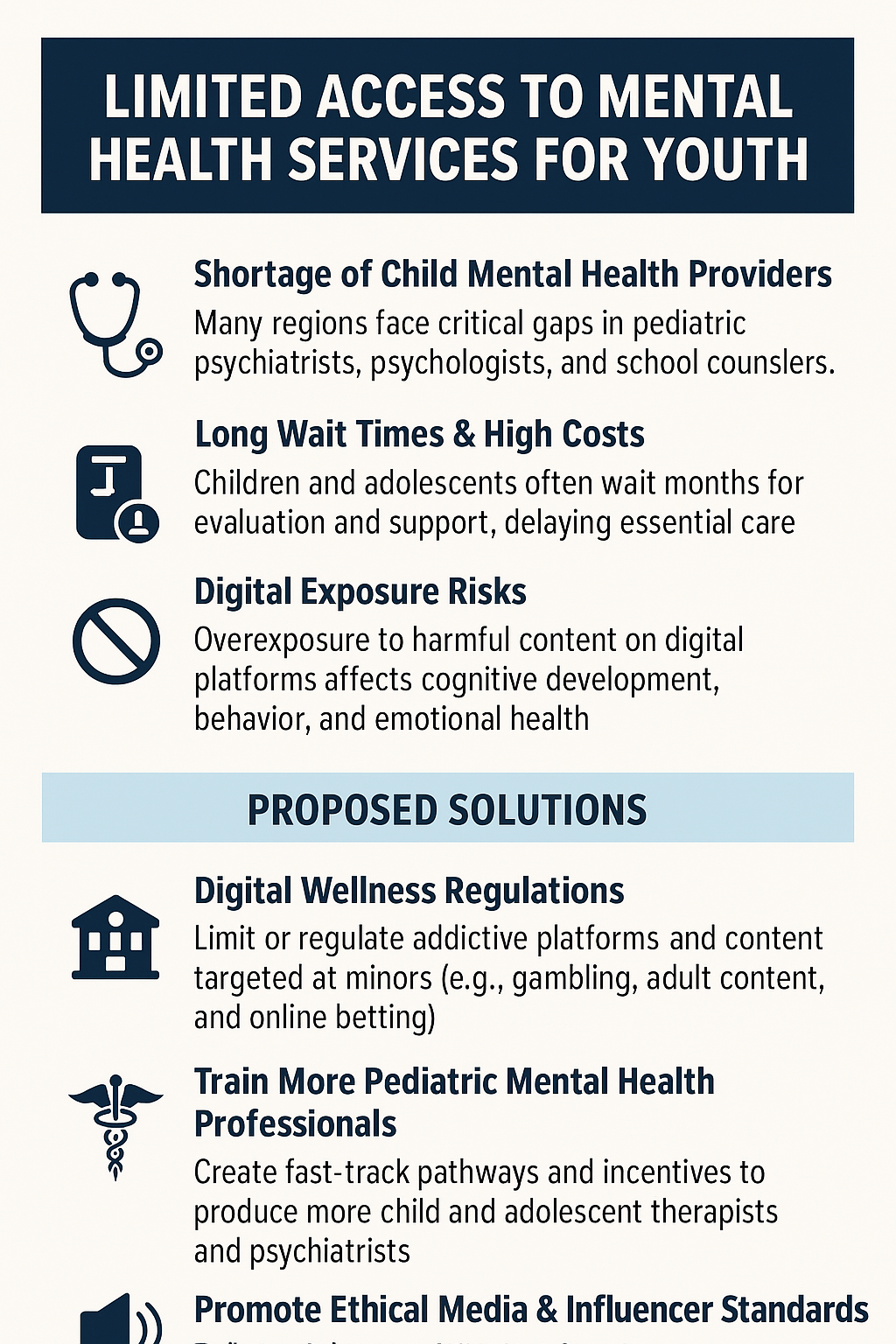
11. Limited access to mental health services (General & Youth)
Inadequate mental health resources, including long wait times and few specialists, impact well-being. This gap requires urgent attention, particularly for youth. Stigma surrounding mental health issues further hinders individuals from seeking care.
Solutions:
- Increase funding and accessibility of mental health services, especially in underserved areas and for youth.
- Integrate mental health care into primary care settings.
- Launch public awareness campaigns to reduce stigma.
- (Youth Specific) Ban harmful social media/online content for minors.
- (Youth Specific) Ban influencer promotion of gambling, porn etc. to minors.
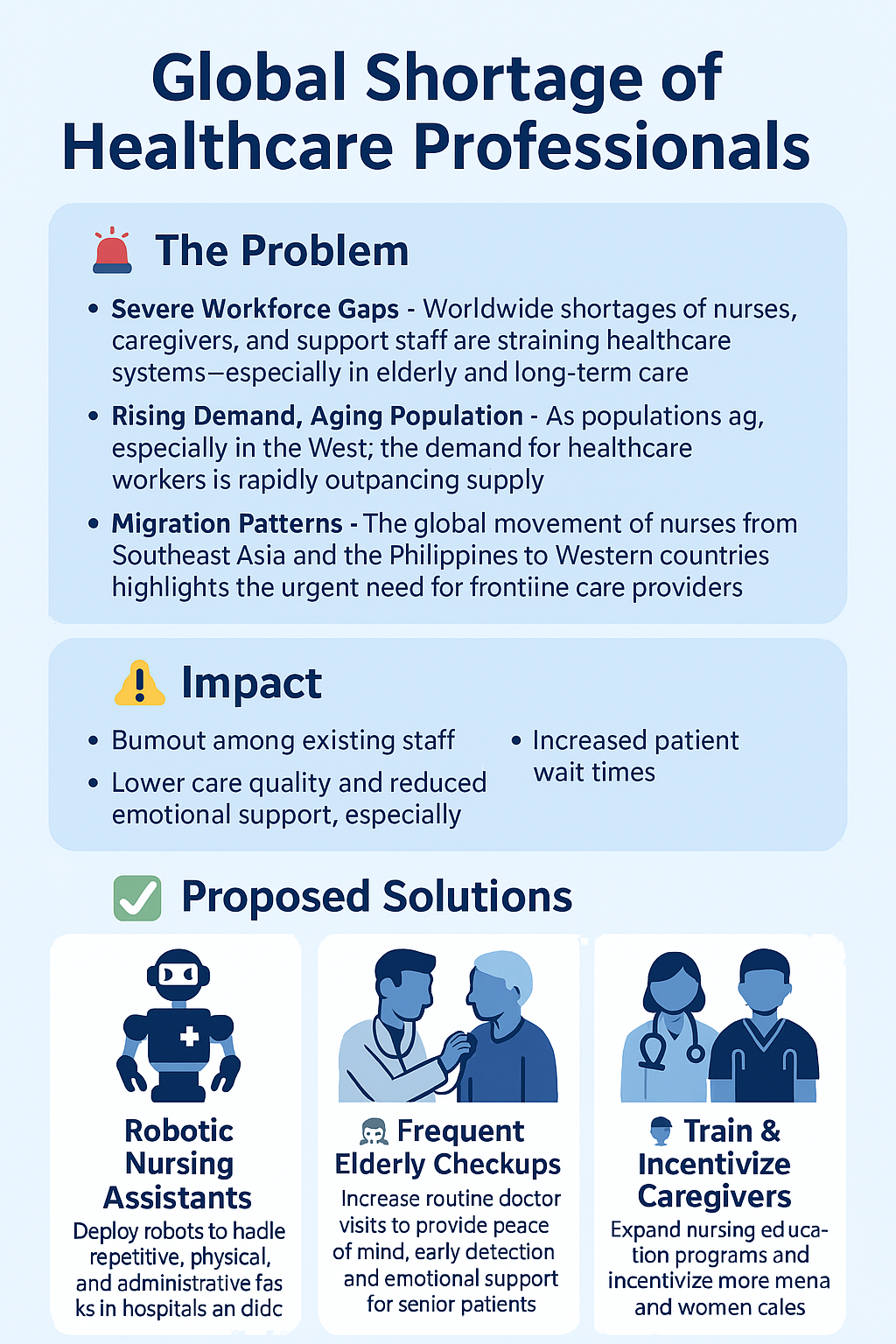
12. Shortage of healthcare professionals
A global deficit of doctors, nurses, and other care workers leads to overworked staff and longer patient wait times. This compromises care quality worldwide. The mass immigration of healthcare workers highlights needs in certain regions.
Solutions:
- Robotic assistance (e.g., robotic nurses)
- Expand training programs for healthcare workers (nurses, providers).
- Streamline immigration/licensing for qualified foreign professionals.
- Improve working conditions to retain existing staff (related to Burnout - #13).
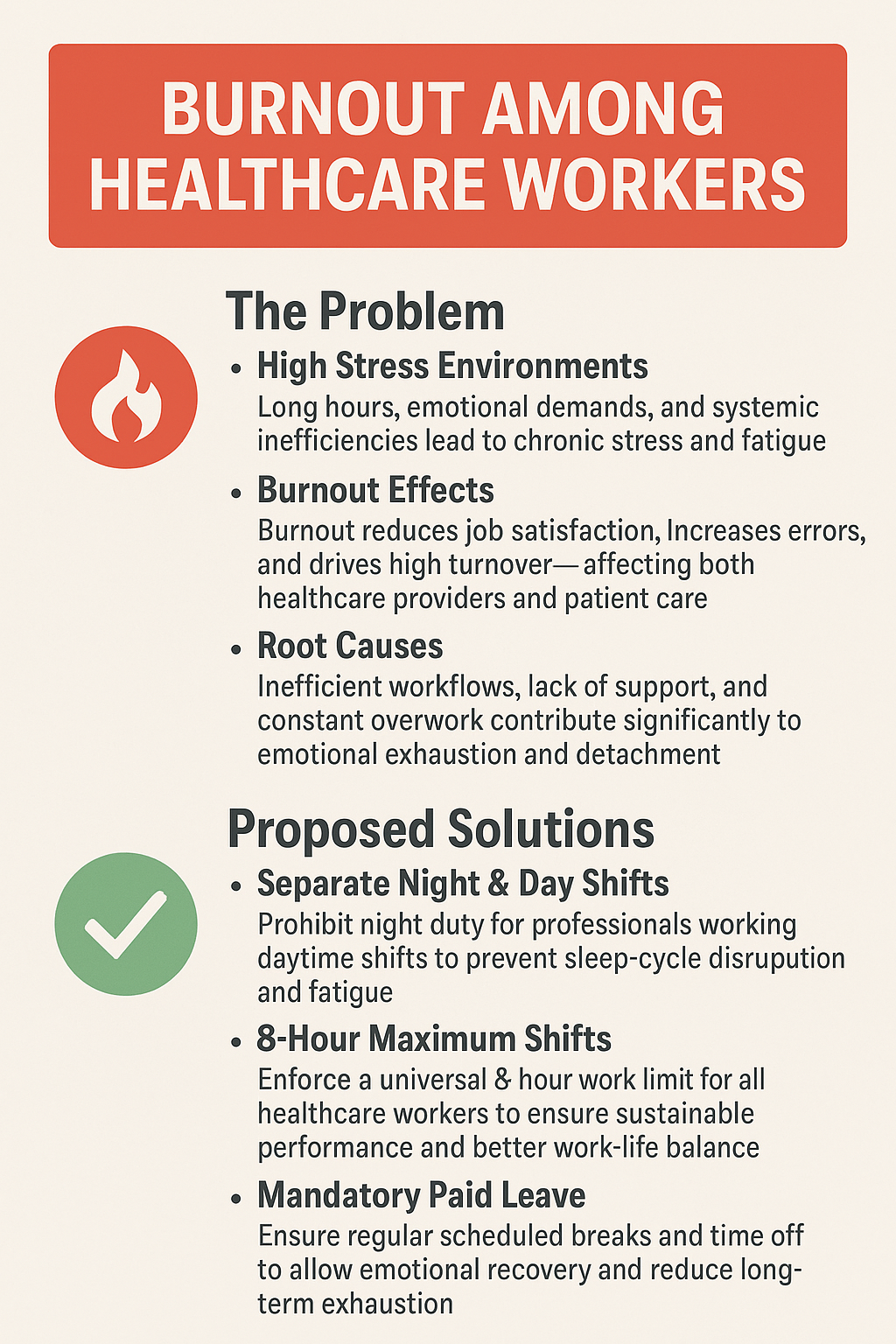
13. Burnout among healthcare workers
Stress, long hours, administrative burden, and emotional tolls contribute to burnout, reducing job satisfaction and increasing turnover. Inefficiency (potentially linked to factors in #1) can exacerbate this. This affects both providers and patients negatively.
Solutions:
- Implement reasonable work hour limits (e.g., max 8-hour shifts).
- Mandate adequate time off and breaks.
- Provide mental health support resources for staff.
- Reduce administrative burdens through better technology/processes (#16, #17).
- Address staffing shortages (#12).
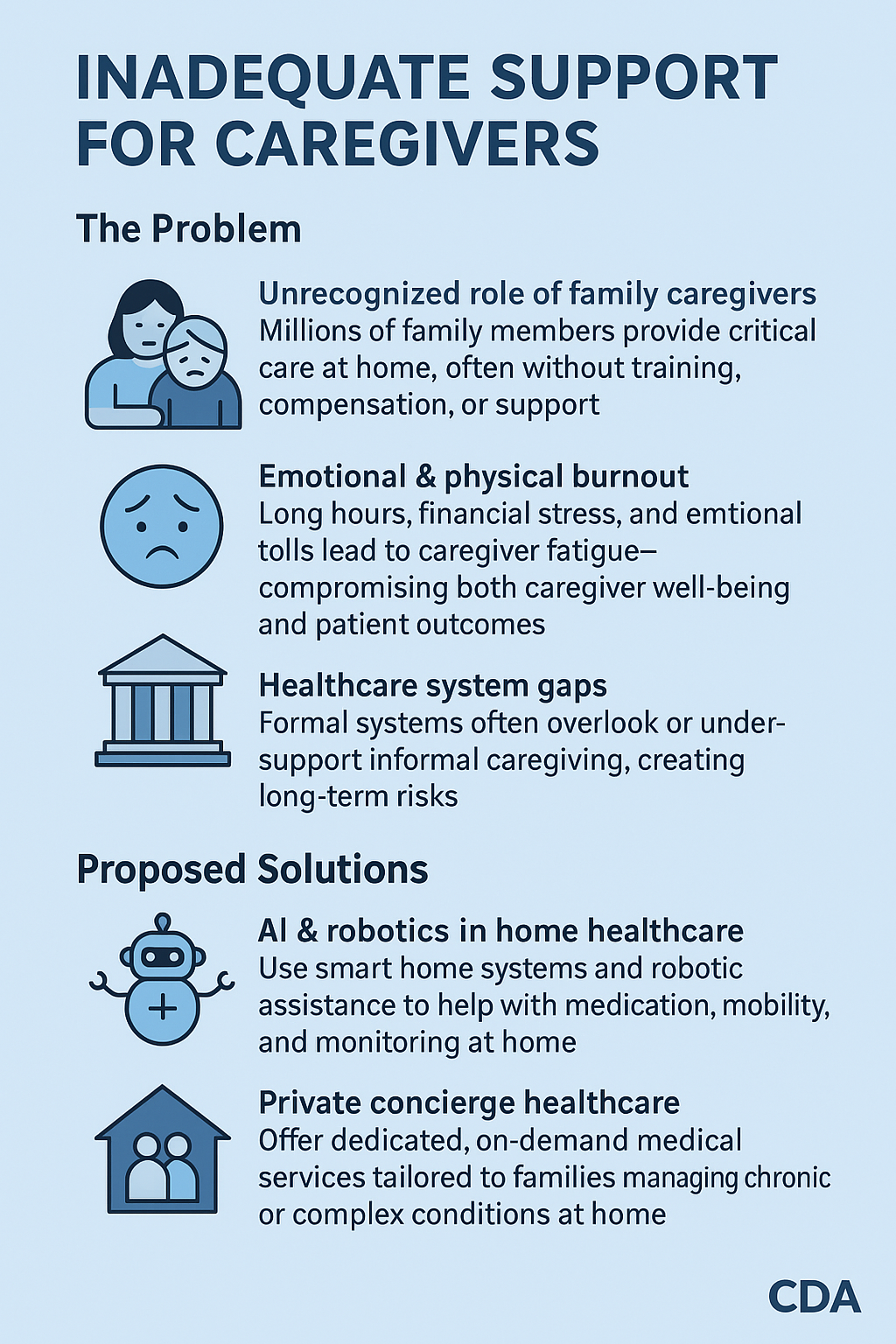
14. Inadequate support for caregivers
Family caregivers often lack sufficient financial, informational, and respite resources, leading to burnout and potentially reduced care quality for patients. Support systems are essential for this crucial group.
Solutions:
- AI-Robotics for home healthcare assistance.
- Expand access to respite care services.
- Provide financial assistance or tax credits for caregivers.
- Offer training and support groups for caregivers.
- Promote policies supporting family cohabitation/care.
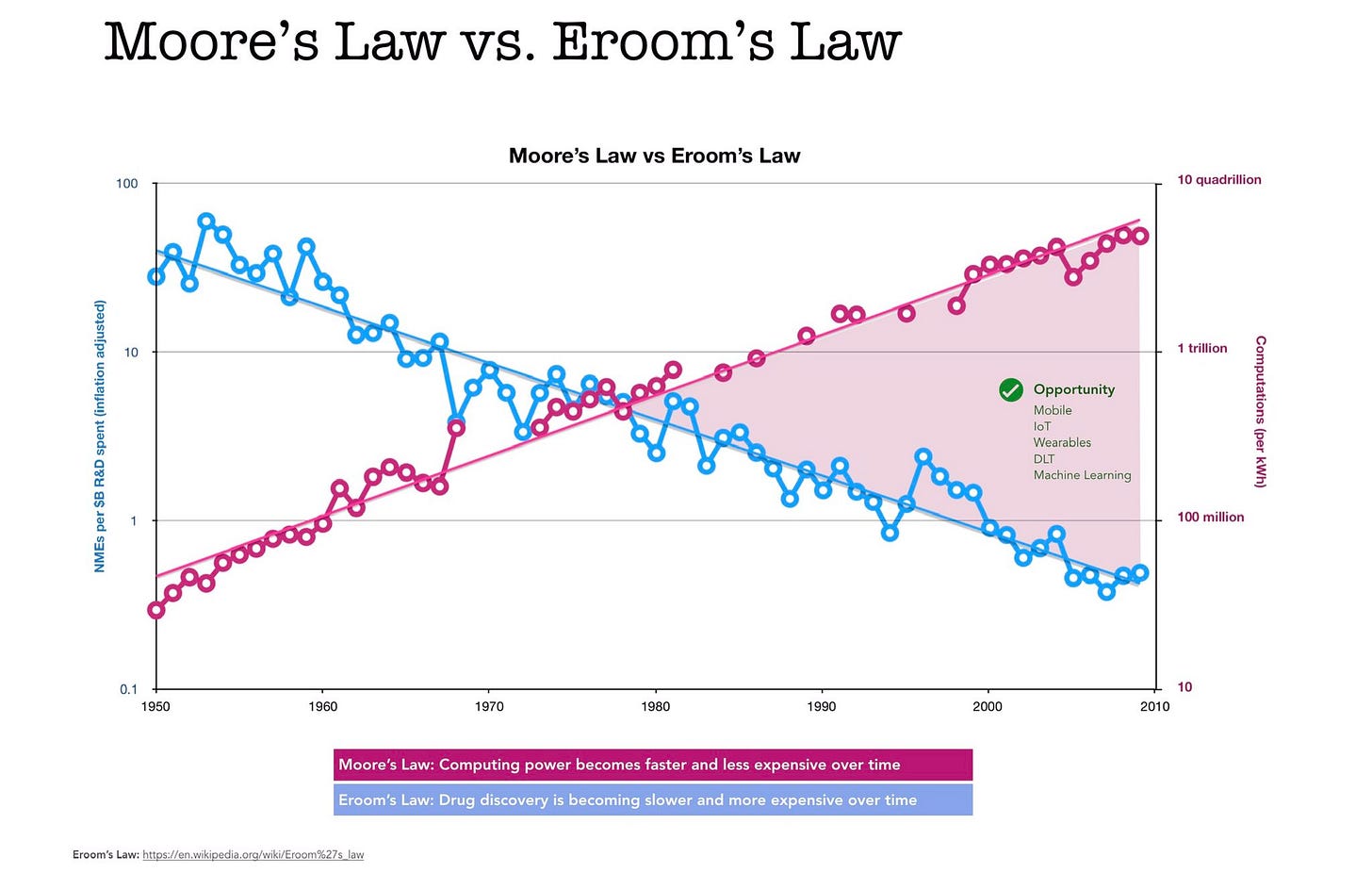
15. Insufficient funding for medical research
Limited research funding slows innovation and the development of new treatments, especially for rare diseases. Concerns exist about the allocation of funds (e.g., pre-clinical vs. clinical research) potentially hindering direct patient benefit.
Solutions:
- Increase overall public and private investment in medical research.
- Prioritize funding for clinical and translational research with clear patient impact.
- Streamline regulatory processes for promising research (#4).
- Explore alternative funding models (e.g., pivoting rare disease drugs towards broader markets like supplements to offset costs).
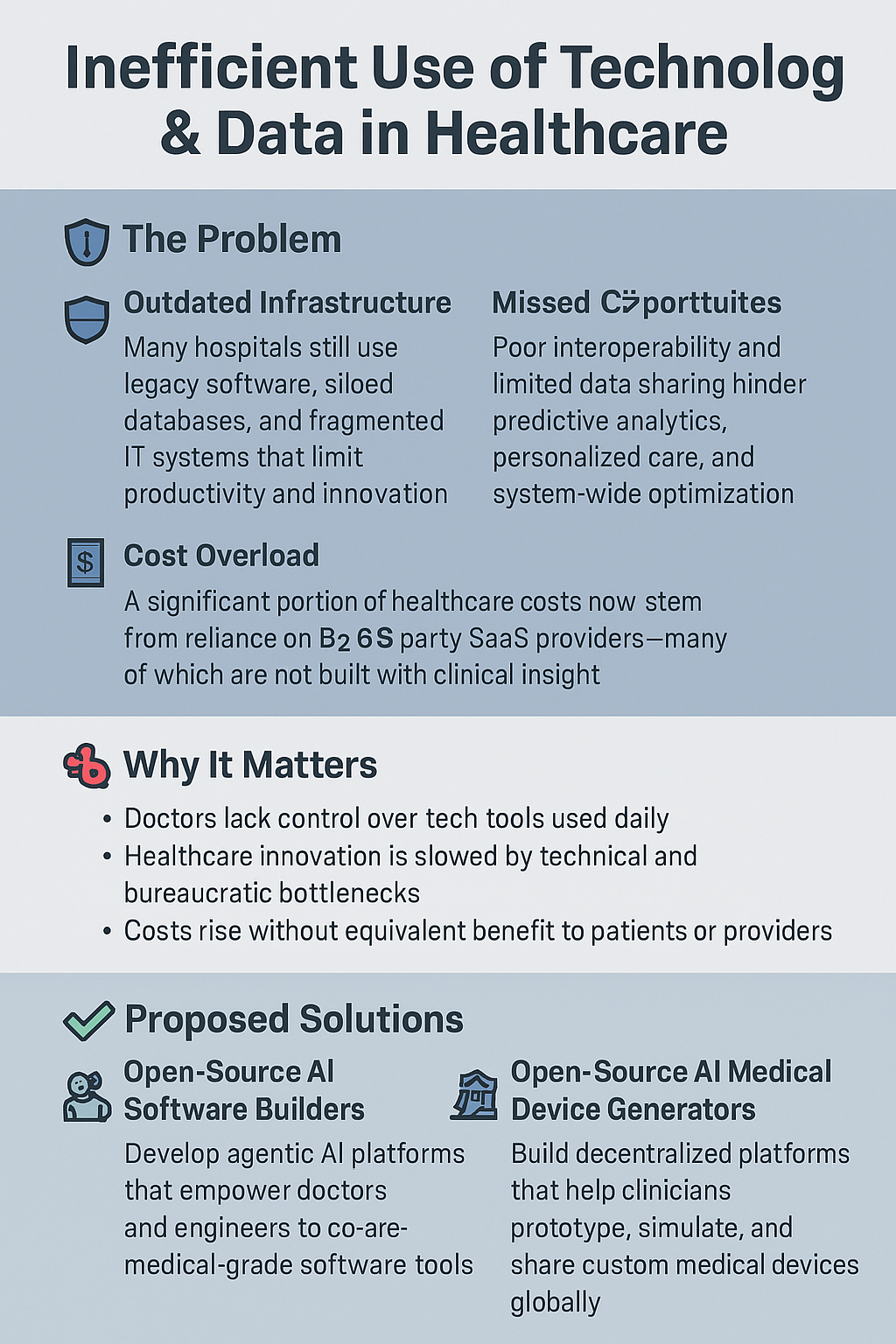
16. Inefficient use of technology and data
Outdated systems, lack of integration (#17), and poor data utilization reduce efficiency, hinder communication, and miss opportunities for improvement and innovation. High costs of B2B SaaS solutions exacerbate this.
Solutions:
- Promote development and adoption of open-source healthcare software/firmware/device designs.
- Invest in modernizing health IT infrastructure.
- Train healthcare professionals in data literacy and technology use.
- Facilitate secure data sharing and analytics for quality improvement and research.
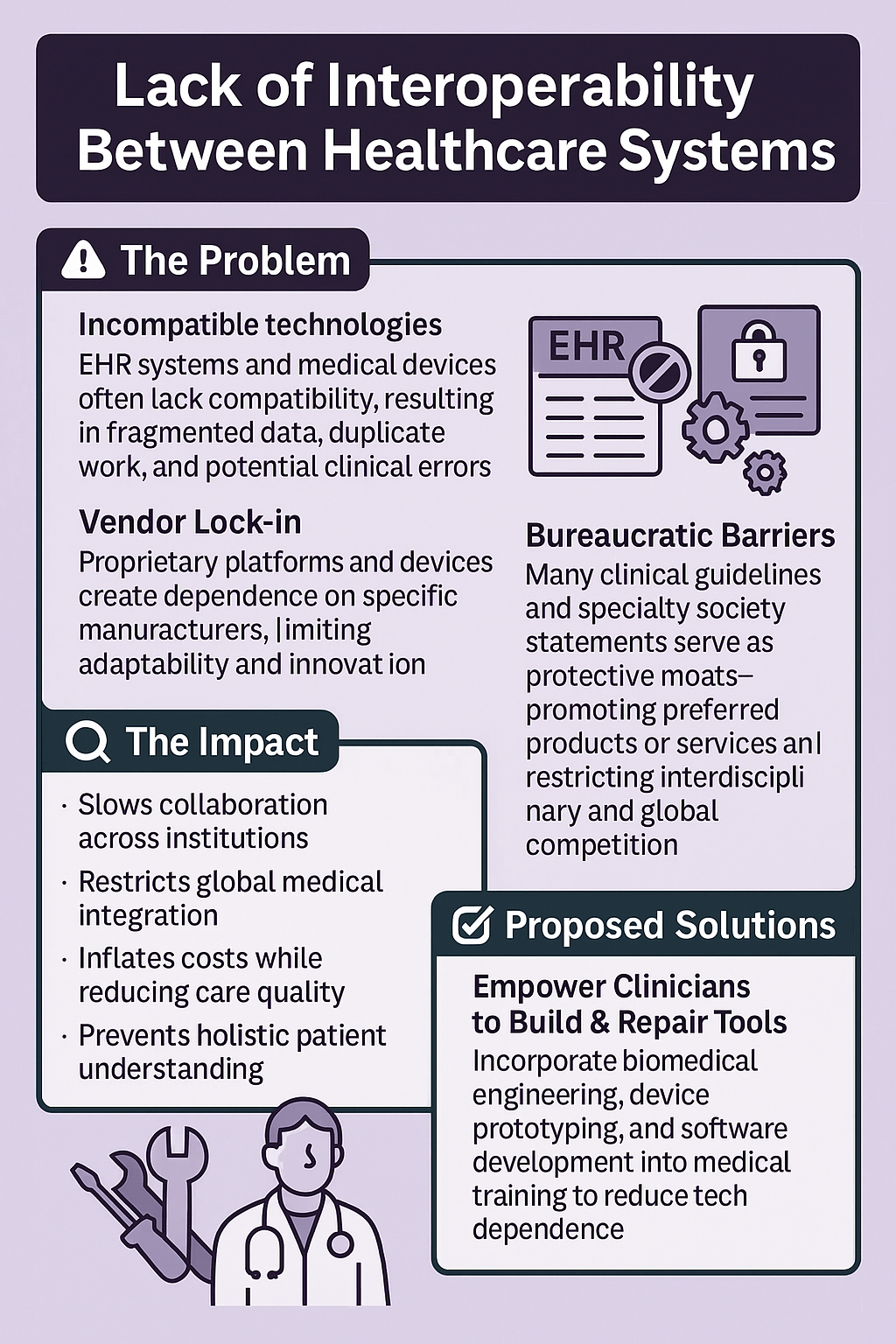
17. Lack of interoperability between healthcare systems
Incompatible technologies (EHRs, medical devices with vendor lock-in) hinder information sharing between providers and systems. This leads to fragmented care, duplicated tests, potential errors, and inefficiency. Intentional "moats" (e.g., non-standard guidelines) can worsen this.
Solutions:
- Mandate and enforce universal healthcare data standards (e.g., FHIR).
- Incentivize or require vendors to build interoperable systems (discourage vendor lock-in).
- Promote open APIs for health data exchange.
- Adopt evidence-based guidelines based on scientific merit, not geography or specific interests.
- Empower patients with control and access to their own health data.
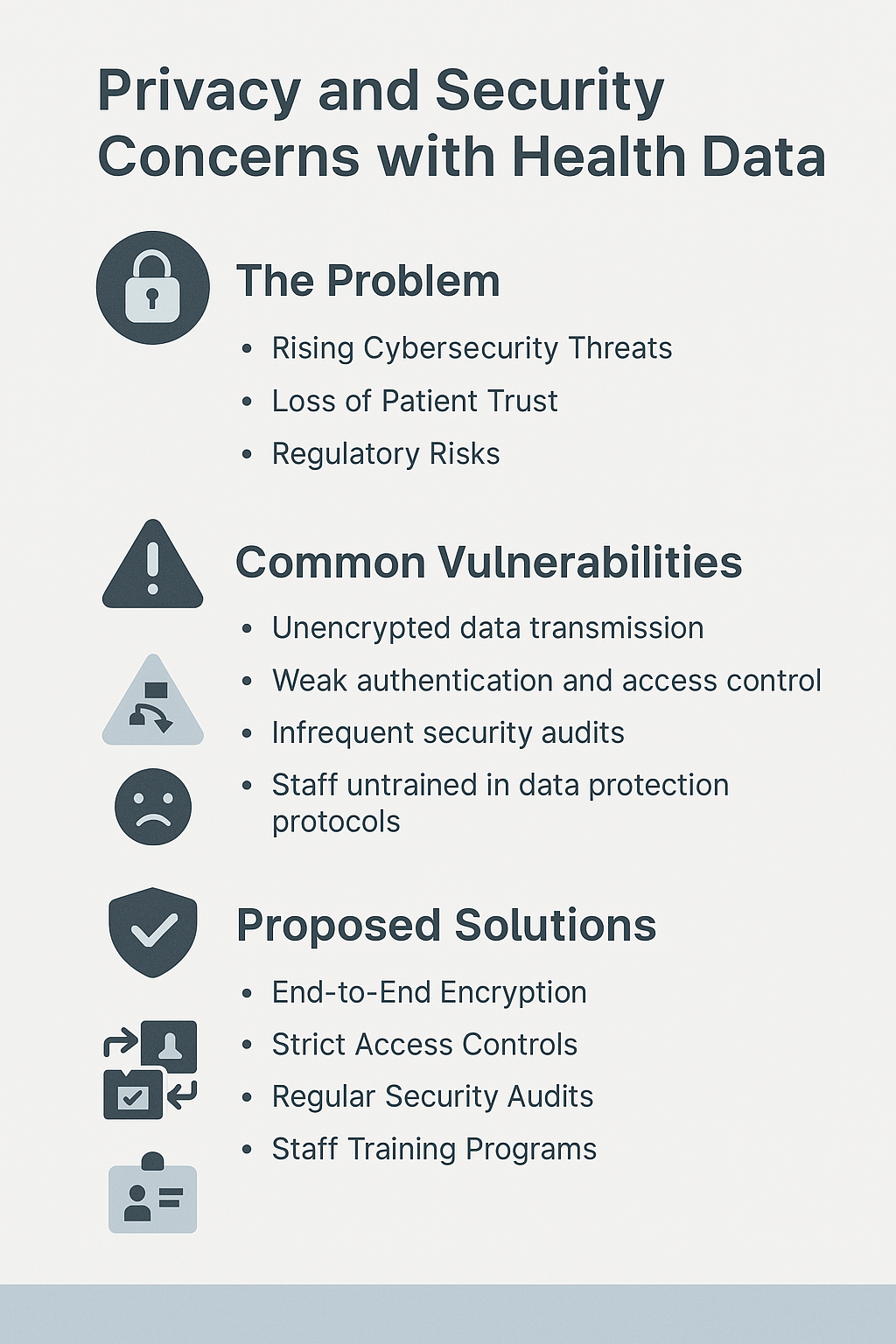
18. Privacy and security concerns with health data
As healthcare becomes more digital, the risk of data breaches and unauthorized access to sensitive patient information increases. This undermines patient trust and poses significant risks.
Solutions:
- Implement robust security measures: end-to-end encryption, strong access controls, multi-factor authentication.
- Conduct regular security audits and penetration testing.
- Provide ongoing security awareness training for staff.
- Utilize privacy-preserving technologies (e.g., de-identification, blockchain for certain use cases).
- Establish clear data governance policies and ensure compliance (e.g., HIPAA).
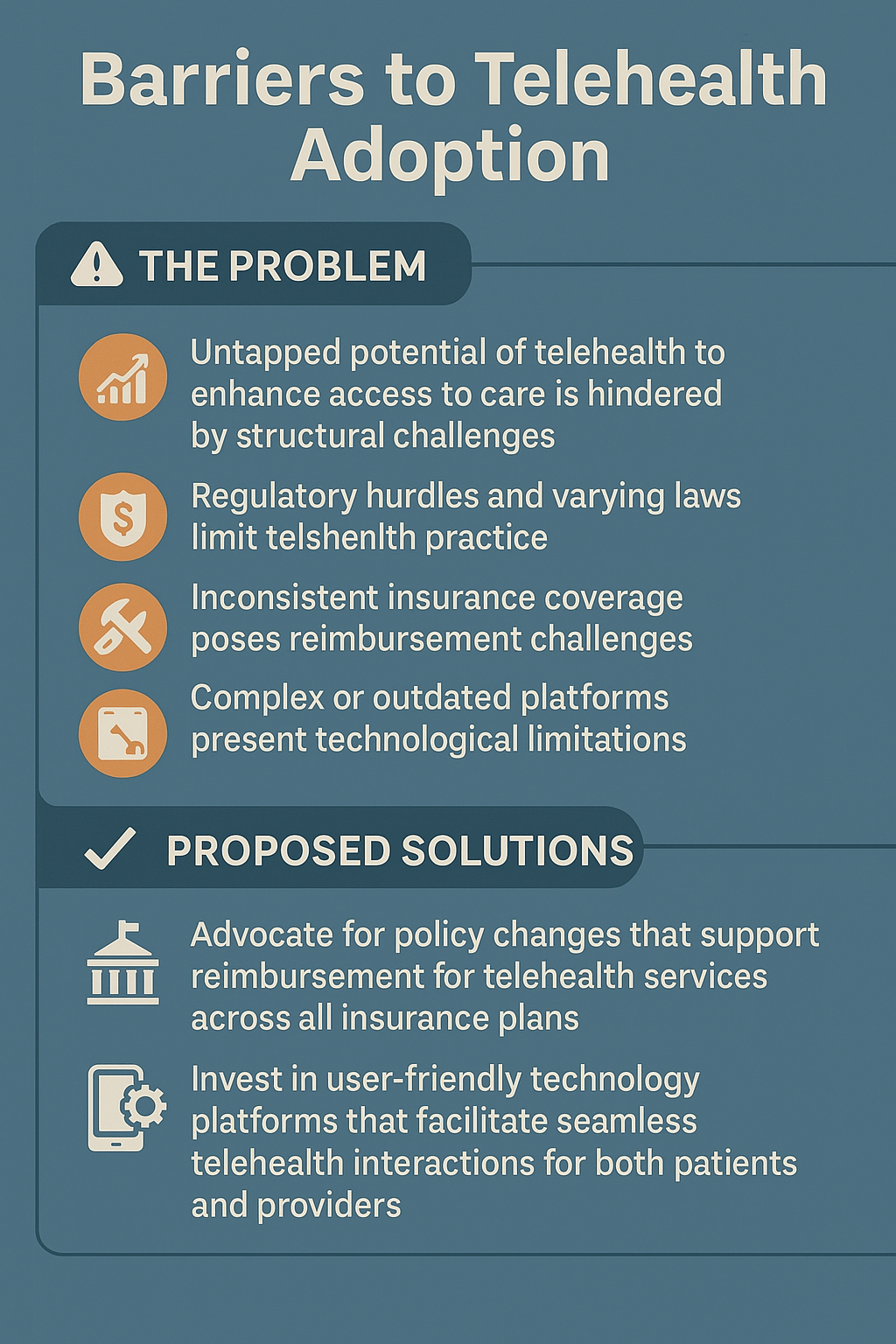
19. Barriers to telehealth adoption
Despite its potential, widespread telehealth adoption faces hurdles including inconsistent reimbursement policies, state licensing restrictions, lack of access to necessary technology (broadband, devices) for some patients, and provider/patient reluctance or lack of training.
Solutions:
- Advocate for permanent, equitable telehealth reimbursement policies.
- Standardize and simplify interstate licensing for telehealth providers.
- Invest in broadband infrastructure and programs to provide devices/digital literacy training for underserved populations.
- Develop user-friendly telehealth platforms.
- Provide training for both providers and patients on using telehealth effectively.
20. Lack of diversity in clinical trials
Underrepresentation of various racial, ethnic, age, and gender groups in clinical trials limits the generalizability of research findings. Treatments may be less effective or have different side effects in excluded populations.
Solutions:
- Implement targeted outreach and recruitment strategies for underrepresented communities.
- Build trust through community partnerships and engagement.
- Provide trial information in multiple languages and culturally competent support.
- Address logistical barriers: offer transportation, childcare, flexible scheduling, stipends.
- Design trials with diversity and inclusion goals from the outset.
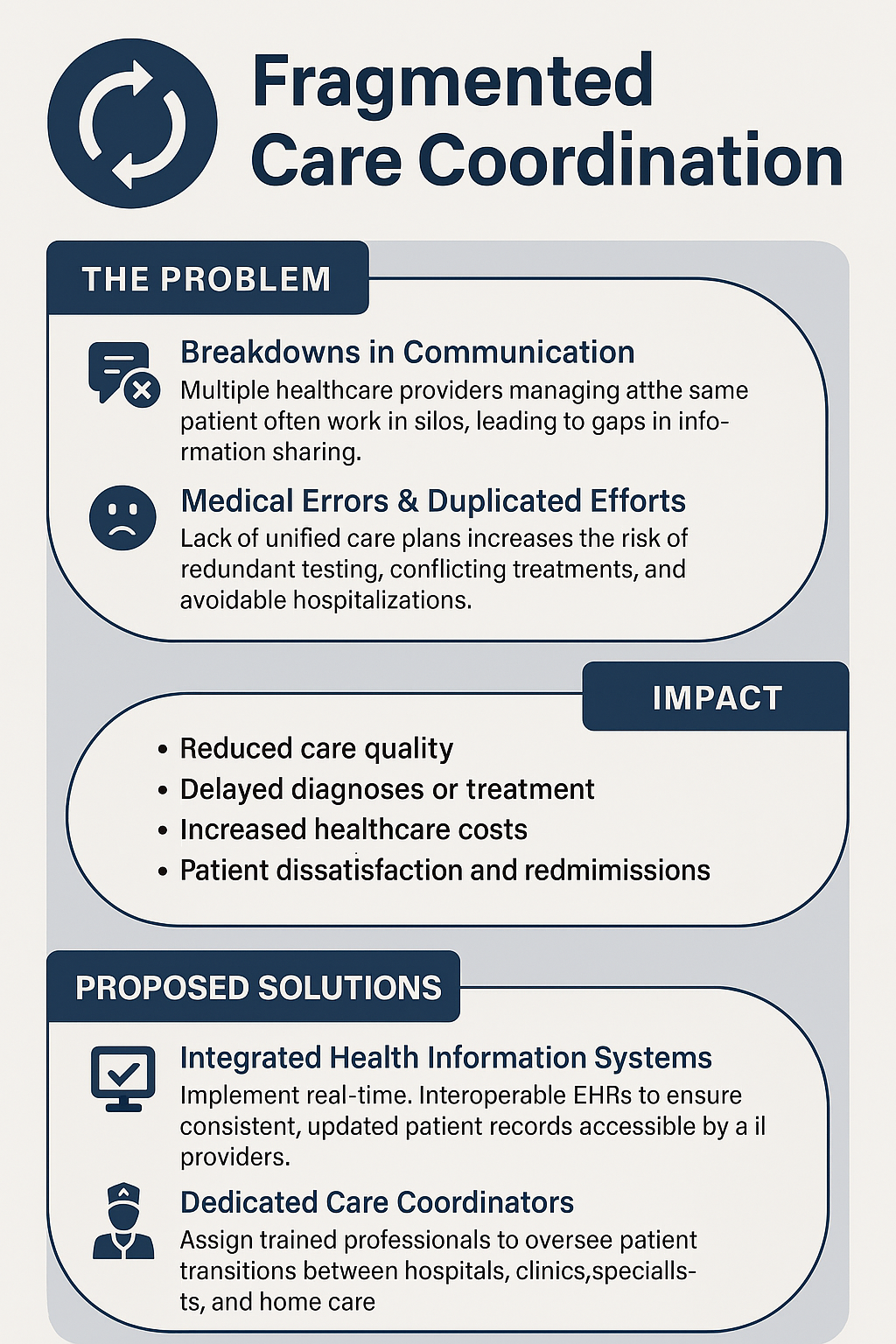
21. Fragmented care coordination
Poor communication and coordination among different healthcare providers (primary care, specialists, hospitals, labs) involved in a patient's care leads to gaps, redundancies, delays, and medical errors.
Solutions:
- Utilize integrated health information systems and shared care plans (#17).
- Employ dedicated care coordinators or patient navigators, especially for complex cases.
- Implement standardized protocols for transitions of care (e.g., hospital discharge).
- Encourage regular communication and multidisciplinary team meetings.
- Empower patients with tools to manage their care and communicate with providers.
22. Antibiotic resistance
The overuse and misuse of antibiotics in human medicine and agriculture leads to the emergence of drug-resistant bacteria ("superbugs"), making infections harder and sometimes impossible to treat. This is a major global health threat.
Solutions:
- Implement antibiotic stewardship programs in healthcare settings to ensure appropriate use.
- Reduce antibiotic use in agriculture and animal husbandry.
- Improve diagnostics to quickly identify bacterial vs. viral infections.
- Invest in research and development of new antibiotics and alternative treatments (e.g., phage therapy).
- Public education on responsible antibiotic use.
- (Advanced) RFID or similar tracking for controlled dispensing.
23. Medical errors and patient safety
Errors in diagnosis, medication administration, surgery, and other aspects of care are a significant cause of preventable harm, disability, and death. Creating a culture of safety is paramount.
Solutions:
- Implement standardized safety protocols, checklists, and best practices.
- Utilize technology effectively: EHRs with decision support, barcode medication administration.
- Foster a non-punitive culture for reporting errors and near misses to enable learning.
- Provide regular patient safety training for all staff.
- Involve patients and families in safety efforts (e.g., asking questions, verifying information).
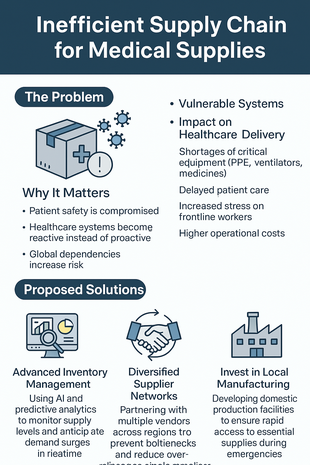
24. Inefficient supply chain for medical supplies
Fragile or inefficient supply chains for essential medicines, devices, and personal protective equipment (PPE) can lead to shortages, especially during public health emergencies or disasters, compromising patient care and safety.
Solutions:
- Improve supply chain visibility and data analytics for better demand forecasting.
- Diversify suppliers and manufacturing locations (including domestic production).
- Maintain adequate stockpiles of critical supplies (strategic national/regional reserves).
- Develop contingency plans for supply chain disruptions.
- Implement advanced inventory management systems (e.g., just-in-time with backup).
25. Lack of standardized care protocols
Variations in clinical practice and inconsistent adherence to evidence-based guidelines across different providers and settings can lead to suboptimal patient outcomes, increased costs, and inequities in care.
Solutions:
- Develop, disseminate, and promote adherence to evidence-based clinical practice guidelines.
- Integrate guidelines and decision support tools into EHR systems (#23).
- Conduct regular audits and provide feedback to clinicians on guideline adherence.
- Offer ongoing training and education on current best practices.
- Incentivize adherence through quality measurement and payment models (#27).
26. Insufficient patient education and engagement
When patients lack understanding of their conditions, treatment plans, or how to navigate the healthcare system, it can lead to poor adherence, worse health outcomes, and increased healthcare utilization. Engaged patients tend to fare better.
Solutions:
- Use clear, simple language and avoid jargon; provide materials in multiple languages/formats.
- Utilize teach-back methods to ensure understanding.
- Encourage patients to ask questions and participate in shared decision-making.
- Provide access to reliable health information resources (online portals, apps, printed materials).
- Offer workshops, support groups, and health coaching programs.
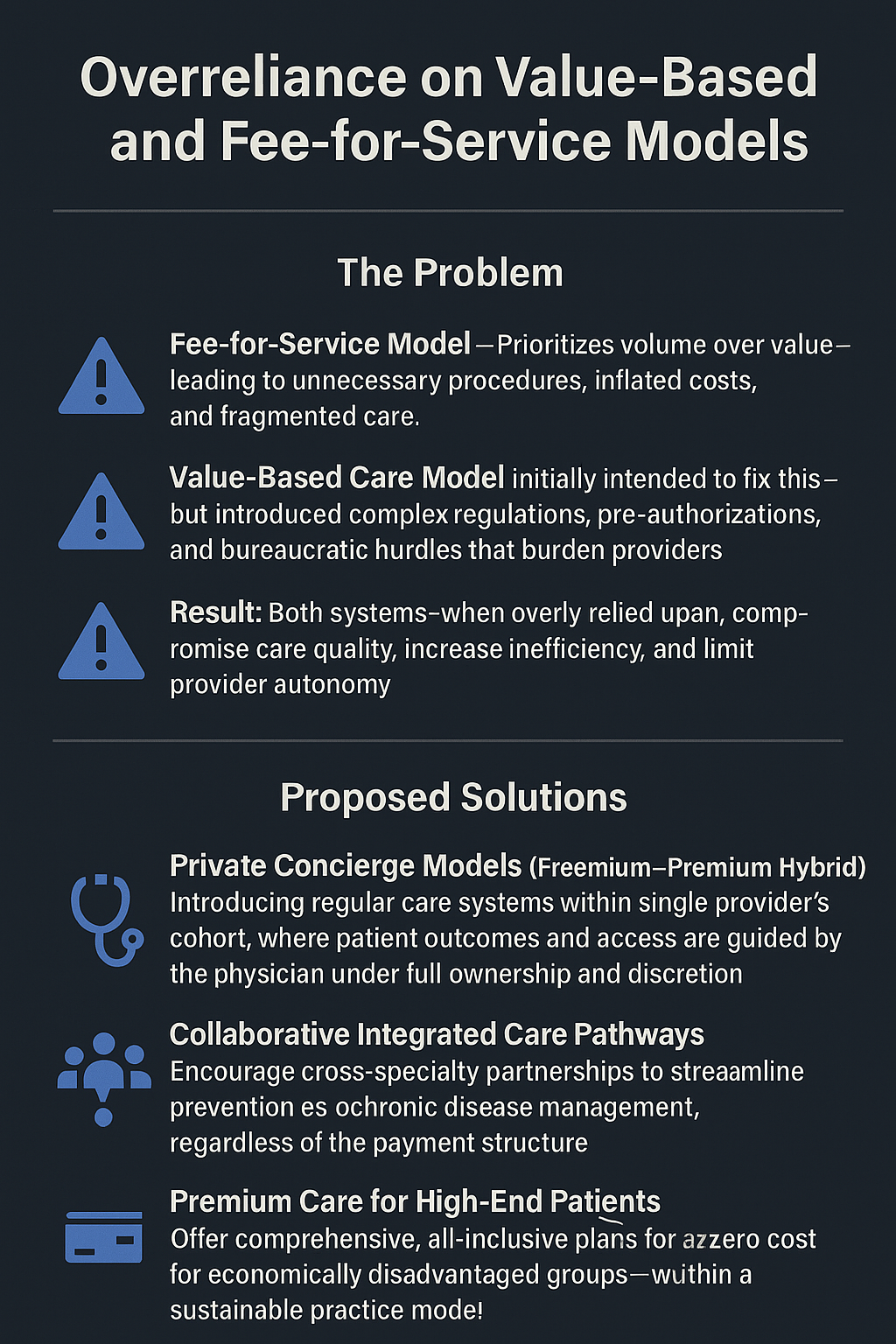
27. Overreliance on Fee-for-Service & Challenges of Value-Based Care
Traditional fee-for-service models incentivize volume over value, potentially leading to unnecessary tests/procedures. While value-based care aims to reward quality outcomes, its implementation can be complex, burdensome (e.g., pre-authorization), and lead to consolidation or restricted choice.
Solutions:
- Refine and simplify value-based payment models to focus on meaningful outcomes and reduce administrative burden.
- Blend payment models (e.g., partial capitation, bundled payments) appropriate to the service.
- Increase transparency in quality and cost data to inform choices.
- Support independent practices and alternative models (e.g., direct primary care, concierge *options*) that prioritize patient relationships.
- Ensure adequate risk adjustment in value-based models.
28. Insufficient focus on preventive care
Healthcare systems often prioritize treating acute illness over preventing disease and promoting wellness. This reactive approach leads to higher long-term costs and missed opportunities to improve population health.
Solutions:
- Train more lifestyle medicine doctors
- Increase funding and insurance coverage for preventive services (screenings, vaccinations, counseling).
- Integrate prevention and wellness programs into primary care.
- Launch public health campaigns promoting healthy behaviors (diet, exercise, smoking cessation).
- Address social determinants of health (e.g., access to healthy food, safe housing) that impact prevention.
- Utilize reminders and outreach to improve uptake of preventive services.
29. Rising rates of chronic diseases
Conditions like diabetes, heart disease, obesity, respiratory diseases, and certain cancers are increasingly prevalent globally. They place a massive burden on individuals, families, and healthcare systems, requiring long-term management.
Solutions:
- Strengthen preventive care efforts (#28).
- More doctors as lifestyle entrepreneurs
- Training AI agents to guide consumer purchase behaiour for health
- Promote healthy lifestyles through private corpoorate policy and niche community programs.
- Improve early detection and diagnosis through accessible screenings with help of AI.
- Enhance chronic disease management programs (education, self-management support, care coordination).
- Address underlying factors like food insecurity, lack of physical activity opportunities, and environmental exposures.
30. Lack of transparency in healthcare pricing
Patients often lack clear information about the cost of healthcare services before receiving them, leading to confusion, unexpected medical bills ("surprise billing"), and difficulty making informed decisions.
Solutions:
- Global pricing on the blockchain acessible through mobile and web apps.
- Mandate clear, accessible price disclosure from providers and insurers for common services.
- Develop user-friendly cost comparison tools for patients.
- Implement regulations against surprise billing (e.g., for out-of-network emergency care).
- Provide patients with good-faith estimates before scheduled procedures.
- Simplify insurance benefit explanations.
Conclusion
These 30 problems illustrate the complexity of healthcare challenges, but they are not insurmountable. Collaborative efforts among policymakers, providers, patients, researchers, and communities can drive meaningful reforms towards a more accessible, affordable, equitable, and effective healthcare system.
References
- World Health Organization: Health Topics
- CDC: Public Health Gateway
- Health Affairs: Health Policy Journal
- KFF (Kaiser Family Foundation): Health Policy
Enjoyed this post?
Subscribe for more insightsFeatured Images